Antimicrobial resistance (AMR) has emerged as a critical global health issue, posing a significant threat to human and animal health, as well as the environment. The rise of resistant microorganisms has been driven by the misuse and overuse of antibiotics and other antimicrobial drugs. As these once potent medicines lose their effectiveness, we are entering an era where simple infections could become life-threatening once again. It is imperative to understand the causes, consequences, and potential solutions to combat this growing crisis.
Table of Contents
What is Antimicrobial resistance?
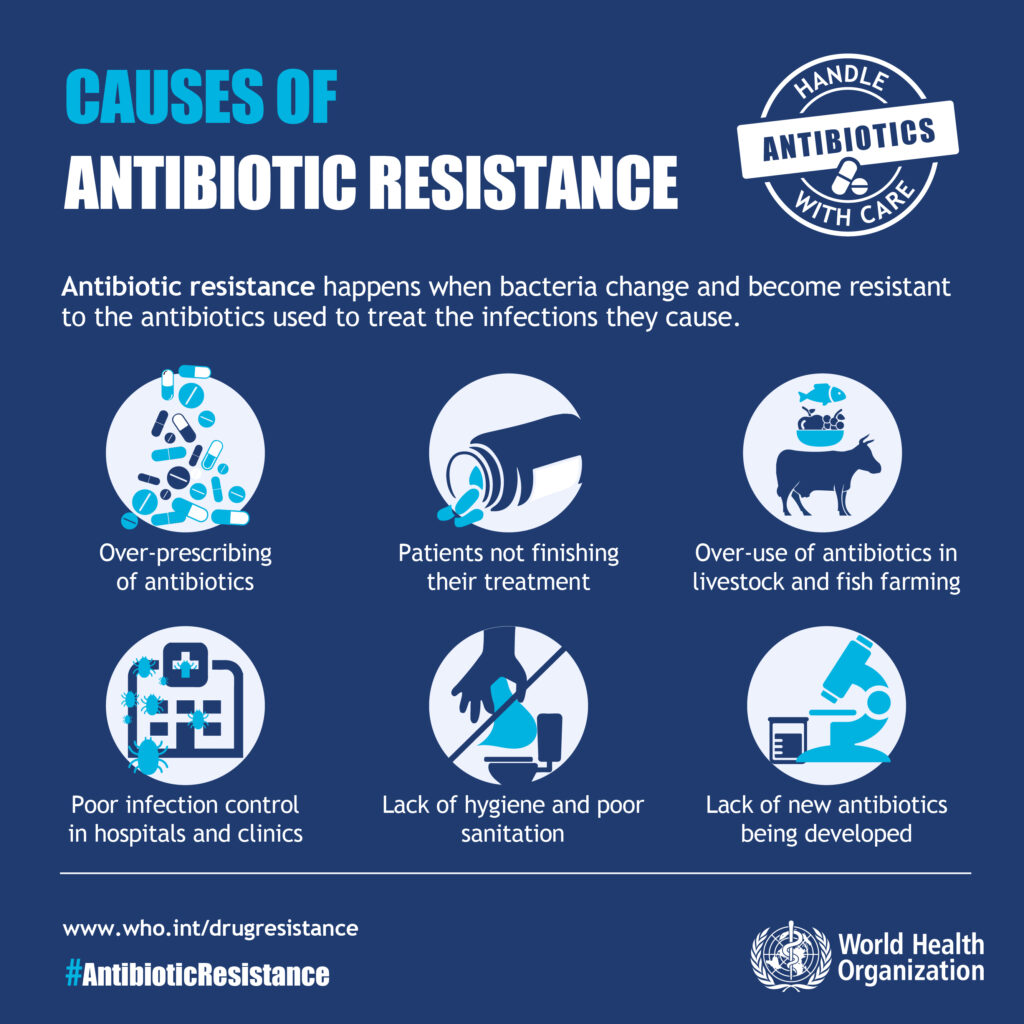
Antimicrobial resistance is the ability of microorganisms, including bacteria, viruses, fungi, and parasites, to resist the intended effects of drugs intended to eliminate or inhibit their growth. Over time, these microorganisms adapt and evolve, rendering the drugs ineffective. The overuse and misuse of antibiotics, both in human medicine and agriculture, are key contributors to the development of AMR. Factors such as incomplete courses of treatment, inappropriate prescriptions, and the use of antibiotics in livestock farming have accelerated the emergence and spread of resistant strains.
Consequences of AMR:
The consequences of antimicrobial resistance are far-reaching. First and foremost, it jeopardizes our ability to treat common infections. Simple ailments like urinary tract infections, pneumonia, and surgical site infections could become life-threatening, leading to higher mortality rates. In addition, the rise of drug-resistant pathogens prolongs hospital stays, increases healthcare costs, and places a significant burden on healthcare systems worldwide. Furthermore, AMR threatens the progress made in modern medicine, including organ transplants, chemotherapy, and complex surgeries that rely on effective antimicrobial agents.
The Environmental Impact:
AMR not only affects human and animal health but also has ecological consequences. Antibiotics and antimicrobial compounds find their way into the environment through wastewater, agricultural runoff, and improper disposal. This exposure creates selective pressure, promoting the growth and spread of resistant bacteria in the environment. The transfer of resistance genes between environmental bacteria and human pathogens adds another layer of complexity to the AMR crisis.
Addressing the AMR Crisis:
Combating antimicrobial resistance requires a multi-faceted and coordinated approach. It begins with improving awareness and education among healthcare professionals, patients, and the general public about the responsible use of antibiotics. This includes promoting appropriate prescribing practices, encouraging adherence to treatment regimens, and discouraging the use of antibiotics for non-bacterial infections.
Furthermore, there is a need for enhanced surveillance systems to monitor the emergence and spread of resistant strains. Countries must prioritize the collection and analysis of data to inform decision-making and track resistance patterns. In addition, it is crucial to invest in research and development of new antimicrobial drugs, diagnostics, and alternative treatments to reduce reliance on traditional antibiotics.
One Health Approach: Addressing AMR necessitates adopting a One Health approach, recognizing that human health is interconnected with the health of animals and the environment. Efforts should be directed towards integrating human medicine, veterinary medicine, agriculture, and environmental sciences to curb the spread of AMR and promote responsible use of antimicrobials.
Policy Interventions: Governments and policymakers play a vital role in combating AMR. Policies and regulations must be developed and implemented to promote rational use of antibiotics, enhance surveillance systems to track resistant strains, invest in research and development of new antimicrobial drugs, strengthen infection prevention and control measures, and improve access to quality healthcare services.
International Cooperation: AMR is a global challenge that requires international cooperation and collaboration. Efforts should be made to facilitate information sharing, research collaboration, and the exchange of best practices among nations. Cooperation between governments, international organizations, healthcare professionals, researchers, and civil society is crucial for developing comprehensive strategies to tackle AMR effectively.
Conclusion
Antimicrobial resistance poses a significant threat to public health, with the potential to reverse many medical advancements achieved over the past century. The indiscriminate use of antibiotics and other antimicrobial drugs has fueled the emergence and spread of resistant microorganisms.
To tackle this crisis, we must prioritize responsible antibiotic use, invest in research and development of new treatments, and promote global cooperation. Only through collective action can we preserve the effectiveness of antimicrobial drugs and safeguard the health of future generations.